What To Do Before You Build That Hybrid OR
Charles Franc

What: The integration of interventional and surgical techniques is demanding a new working environment for an interdisciplinary cardiovascular team: the Hybrid Operating Room, where angiographic imaging capabilities are integrated in an operating suite.
Essentially, these operating rooms combine the imaging capabilities of a traditional cardiac catheterization laboratory with the function of a cardiac operating room. They can be developed in the operating room setting or in the cath lab setting.
A strict definition of a hybrid procedure is a major procedure that combines a conventional surgical component, including a skin incision, with an interventional component, using a catheter-based procedure guided by fluoroscopic or MRI imaging, in a hybrid room without interruption. Wider definitions include procedures in which the interventional and surgical elements are done in sequence, a surgical technique is only necessary in case of an emergency, or even minor procedures, such as venous cut downs. Sometimes, fluoroscopy guided interventions performed by surgeons (e.g., endovascular aortic repair in aortic abdominal aneurysms) are referred to as hybrid procedures.
Why: Although open heart surgery continues to be the generally preferred method for treating most structural heart disease,[1] interventional techniques can provide a viable alternative for patients for whom conventional surgery is considered to be too risky – and offers the potential benefits of less scarring, blood loss and pain, and a quicker recovery. Catheter-based treatment is a rapidly growing approach to structural heart conditions and is considered by many to be a key component of the comprehensive heart program of the future.
But don’t forget: While the most publicized treatment requiring a hybrid OR is TAVR – Transcatheter Aortic Valve Replacement – your hospital may not qualify through CMS or the device manufacturers (who require specific volume thresholds, as well as many other factors) to perform TAVR. However, there are many other procedures that can be done more effectively and efficiently in a hybrid environment, and these uses may readily justify the expense of developing a hybrid room. These procedures cross many specialties, including cardiothoracic, vascular, orthopedic and other disciplines.
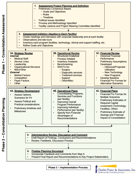
So what do I do? Before a knee jerk reaction (We can’t justify a hybrid room because we won’t be doing TAVR, or We should have one because it’s the thing to do), put the decision through a formal process:
- Interview your physicians (including all possible specialties that might benefit from hybrid capability) to determine what types of procedures would be performed in the hybrid OR. Then answer the following questions:
- Will we be adding additional types of procedures that currently are referred to our competitors – is a market share gain possible?
- Is there enough volume in our potential capture area to drive a responsible financial decision?
- Would a hybrid room allow us to provide better value to our customers – would it improve our marketability to the insurance community?
- Specifically address TAVR. Start with the level of interest on the part of your cardiologists and CT surgeons. If there is interest, is there capability on the part of your physicians? Can this capability be developed through recruitment or through training? Be sure to know the current CMS and device company requirements, as these requirements are evolving.
- Compile a comprehensive listing of procedures that could be done in a hybrid OR. What are the current and future volumes? How will technological changes impact future usage? How many are being performed currently by your facility versus in the market? What is the reimbursement?
- Determine where the hybrid room would best fit in your facility. It could be in your operating room suite or your cath lab suite. Consider the cost and functionality of each option. It is reasonable to assume that any existing main surgery-based solution will be significantly more expensive than a cath lab-based solution, all other factors being equal.
- Complete vendor selection, architectural planning and budget for construction and major capital equipment. Who will provide the major equipment and at what cost? How will the function be integrated into the optimal site option? Preliminary designs will need to be completed to plan and cost the project.
- Develop a financial feasibility assessment and business plan. Using all collected information, is the project strategically, operationally, clinically, politically and financially feasible? What is the business plan for assuring the success of the venture?
- Secure required internal approvals. With all planning complete, what is the internal process of securing authorization to proceed with projects of this type?
- Write a marketing and communications plan. How will the project be best communicated to target audiences to insure its optimal utilization and acceptance in the marketplace?
- Procure the required staff resources and complete training. What new staff will be required? How will they be trained to handle new procedures?
- Implement the program and provide ongoing management. What else needs to be done to insure successful implementation? How will the program be managed on a going-forward basis?
Successful completion of these steps will help to insure the program is feasible, effective and well planned.
As always, CFA invites your comments, questions and suggestions. We also welcome you to download our free eBook series on Strategic Marketing for the Cardiovascular Service Line.
[1] Structural heart diseases affect the heart muscle and the valves that regulate blood flow within the heart. Some structural heart diseases are congenital (born with); others are the result of heart disease or wear on the heart, vessels and valves over time (acquired). Until recently, abnormalities in the structure of the heart required open surgery to repair – surgeries that can cause the patient a great deal of discomfort, have measureable complication and mortality rates, and can require a lengthy recovery time. With the advent of new techniques, interventional cardiologists, working with their cardiac surgery colleagues in many cases, can now perform minimally invasive versions of many of the procedures to repair these disorders.
Related Posts
Effective Planning for Cardiovascular Services Consolidation
John Meyer, FACHE
The issue of consolidation of services between hospitals within a system is increasingly important...

