What To Do Before You Build That Hybrid OR
What: The integration of interventional and surgical techniques is demanding a new working...
The issue of consolidation of services between hospitals within a system is increasingly important and many health systems are evaluating this option.
CFA has heard from several hospitals that are contemplating the consolidation of cardiac surgery into one or more hospitals – most typically, from a community hospital to a “regional” hospital. Consolidation, merger or “rationalization” decisions are complex, and have significant strategic, practical, clinical, financial as well as political ramifications. Most commonly, cardiovascular services consolidation focuses on cardiac surgery, but has implications for other interventional and non-interventional cardiology services as well.
When facing a consolidation opportunity, it is important to have a methodology and approach to the process; after all, these are complex and impactful decisions. We begin by referring you to a previous CFA blog post Are You Considering Consolidating (Rationalizing) Clinical Services Across Your Health System? Consider these 12 Key Questions1.
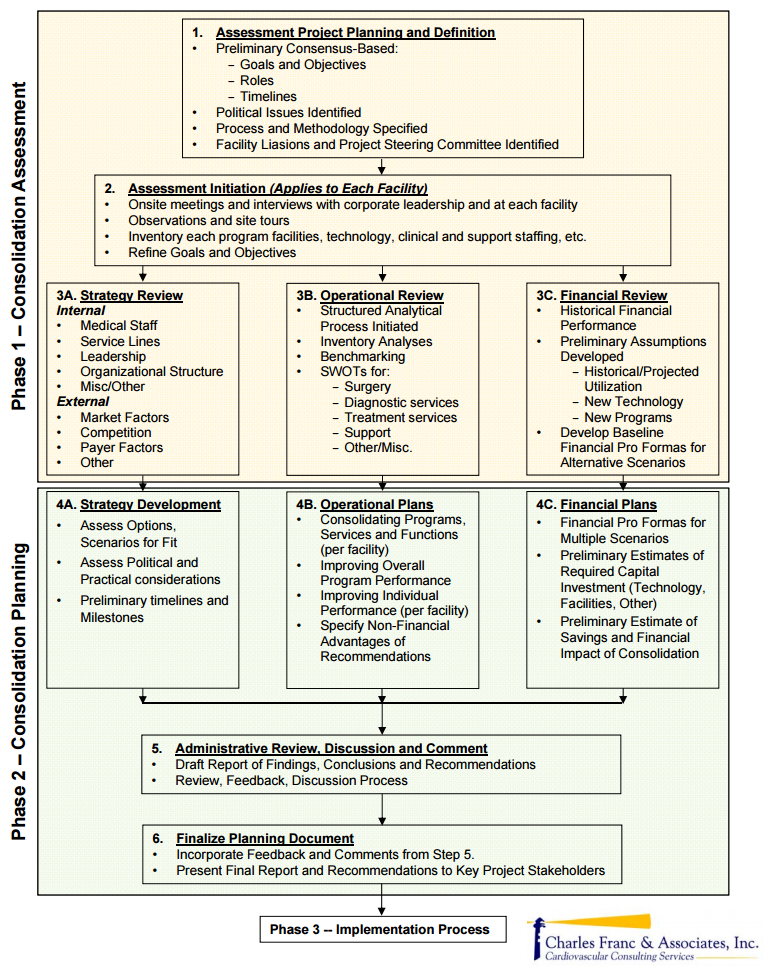
Reviewing this blog will help to frame the issues and focus on the critical questions that serve as the basis for any consolidation analysis and discussion. Keeping these questions in mind, we have developed a three-phase approach to assessing (Phase One), planning (Phase Two) and implementing (Phase Three) a consolidation project. In this blog, we will focus on the Phase One work, assessing the consolidation opportunity, as it gets to the heart of the operative question: should you consolidate service “A” into service “B” at another facility?
Reaching this “go/no-go” decision will obviously be required before definitive planning can take place for an optimal operational entity incorporating service “A,” including what will need to happen to make this change both a reality and a success going forward. These issues constitute Phases Two and Three. Refer to our graphic illustration: CFA 3-Phased Health System Clinical Program Consolidation Process Overview outlining all three phases. Note that every situation is unique; we have tried to simplify the process and its component parts to promote clarity.
Phase One Consolidation Assessment consists of three large blocks of interrelated activities, each of which is summarized below:
3A. Strategy Review – It is critical to understand the internal and external strategy of the facilities and how any redistribution of programs or services may change (positively or negatively) overall performance in the marketplace. An internal review should focus on medical staff, service line offerings, leadership, organizational structure and other related issues. Perhaps more importantly, an external market assessment needs to focus on potential market reaction to changes in service, including target population, competitor, and payer community perceptions and potential reactions. Understanding the consequences of consolidation decisions on a strategic level is just as important as understanding based on clinical, operational or financial impact.
3B. Operational Review – Having built an understanding of each impacted service and facility, the nuts-and-bolts assessment focuses on operational issues to answer the question, “What is the real operational impact of moving a specific service to another facility?” This might involve physician referral patterns or preferences; changes in volumes, staffing patterns, or hours of operation; facility or capacity impacts; changes in performance; clinical outcomes; etc. Cardiovascular programs are complex and have many interdependent pieces – change one and others can change as well. Some changes can be anticipated and planned for; others will be unintended and unanticipated.
3C: Financial Review – Besides strategic, operational and clinical issues, financial assessment is critical and will serve as a strong basis of any “go/no go” decision making. Historical utilization and financial performance will need to be established, and appropriate financial assumptions developed on a going forward basis. For example, if the hospital(s) consider Medicare’s mandatory cardiac bundle as a highly-likely financial scenario, then the analysis should take this into account, both from strategic and financial perspectives2. Financial pro formas will need to be developed for each affected site and for each scenario contemplated; for example, both with- and without the service being assessed. It is important that appropriate assumptions are considered, including volumes and costing, and potential unknowns or contingencies such as “leakage” of referrals if a service is moved from one hospital to another. Additionally, alternative scenarios may need to be considered, and appropriate financial planning done, if there are alternative options that figure into the analysis.
At the completion of the First Phase of the Assessment, the consolidation question should be reasonably well understood and the pros and cons well defined. Recommendations for going forward can be made:
Clear-cut conclusions based on systematic analyses are possible, but a more nuanced approach, weighing all critical factors, is a more likely required outcome. The overall process used to assess consolidation needs to be well thought out, thorough and capable of withstanding criticism of preconception, bias or lack of appropriate input from stakeholders.
If the decision is made to accept the recommendations of the assessment Phase, then the next two phases of work, Consolidation Planning and Implementation, can commence.
Answering these and other logical questions during the analyses and debate over potential cardiovascular services consolidation (or consolidation of other service lines) between facilities is a critical exercise that will help to insure a rational, politically acceptable and well planned outcome. While we as an industry may be well past the full-service hospital fixation, financial and strategic reality will force hospitals to make decisions that will impact their deployment of programs and services (and ultimately, the consolidation, merger, rationalization, or right-sizing thereof) in a more far-reaching way than has ever happened before. CFA believes that when Medicare mandatory cardiac bundled pricing comes to pass, this single event will push many hospitals/health systems to seriously consider consolidation options for the very first time.
If you are interested in learning more about programmatic consolidation for cardiovascular or other services, please contact CFA at (949) 443-4005 or by e-mail at CFA@charlesfrancassociates.com. Our Three-Phased approach to clinical program consolidation can assist hospitals in working through these complex and impactful decisions. See more at http://www.charlesfrancassociates.com/consolidating-cardiovascular-clinical-services.
Download: CFA 3-Phased Health System Clinical Program Consolidation Process Overview
1It should be noted that these questions pertain just as well to any specialty program or service line and not just cardiovascular services.
2Forming a single hospital program that can offer competitive bundled pricing, higher volume and better outcomes may be more advantageous than offering two hospital programs with bundled pricing where each hospital features less-than-competitive performance and outcomes.

What: The integration of interventional and surgical techniques is demanding a new working...

In the continuing effort to foster innovation and cost savings in cardiovascular programs, CFA was...