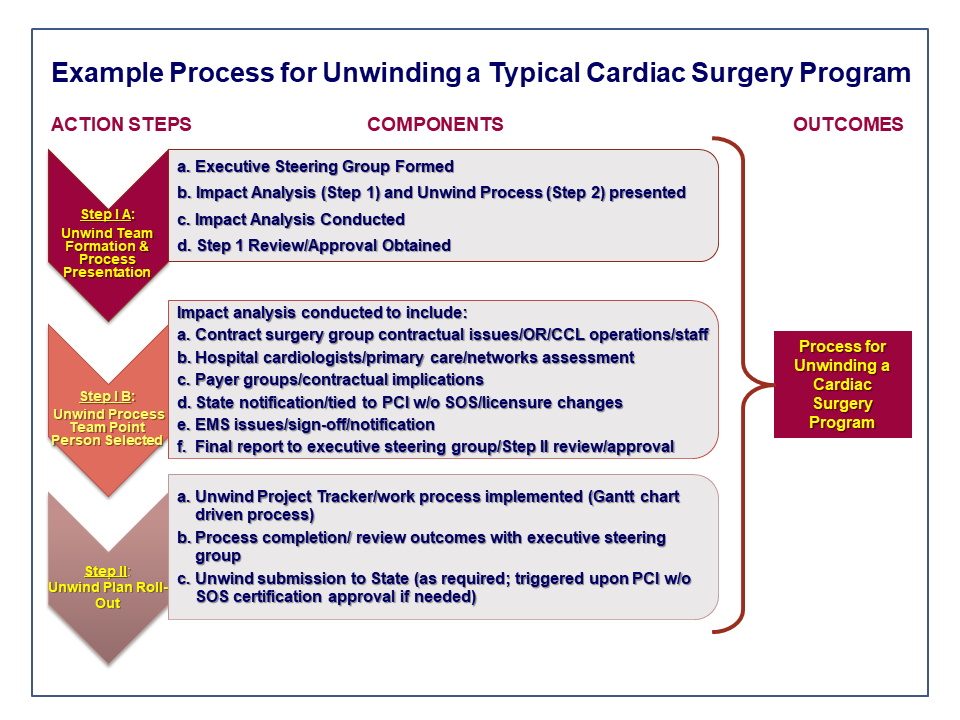
In our continuing series on low-volume cardiac surgery program issues and strategies, we thought it would be beneficial to present a conceptually simple and straightforward methodology and approach to “unwinding” a program should that be the decision of hospital management and clinicians. Having conducted this process with clients on occasion, it represents a way to comprehensively prepare for and efficiently and effectively divest a cardiac surgery program, with special emphasis on the operational implications inherent in such an endeavor.
Assuming that a decision has been made to stop providing cardiac surgery either altogether or through affiliation and/or consolidation with another clinical provider (please see our blog on the consolidation issue here), it is important that the implications of such an action be fully considered and systematic steps be taken to both lessen the potential negative impact on the organization and compensate for this by solidifying other aspects of the overall cardiovascular program. In many cases, this “compensation” will involve (depending upon the specific state) receiving licensure or certification to offer PCI without on-site cardiac surgery. In California, this can involve a lengthy and somewhat complex application and certification process, and includes designating a referral hospital for cardiac surgical transfers, but each state situation will vary. The process we have successfully used encompasses three major steps (refer to graphic) inclusive of a number of logical component parts, as summarized briefly below.
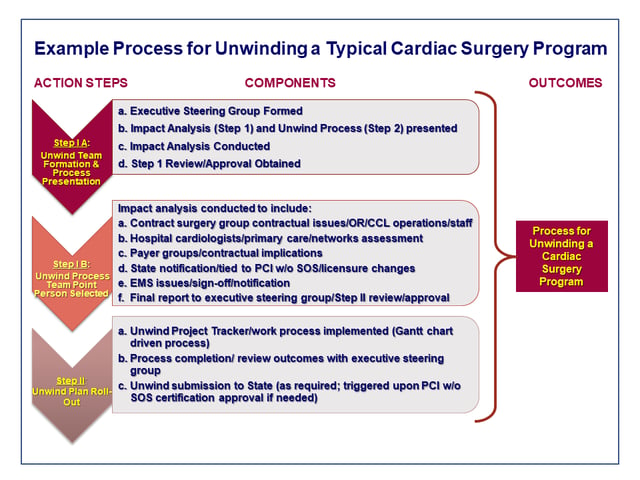
Step One A: Unwind Team Formation and Process Presentation
The first step consists of the appointment of an Executive Steering Group (ESG) to oversee the process and approve all necessary actions required to initiate the unwinding. An Impact Analysis (IA also Step 1) needs to be conducted and an Unwind Process (UP also Step 2) designed. The IA is designed to identify all of the relevant positive and negative impacts such an action will cause, and consideration given to consequences and action required to mitigate these consequences. Additionally, a Team Point Person will need to be identified and selected.
Step One B: Unwind Process/Team Point Person Selected
The IA designed in Step One A is initiated in Step One B. The IA is designed to identify all of the relevant positive and negative impacts such an unwind action will cause, and consideration given to consequences and action required to mitigate these consequences as may be required. Upon initiation, and as needed, unintended consequences need to be identified in real time and presented to the ESG for prompt resolution through the designated Team Point Person. An important factor is the identification of long lead-time items, such as necessary changes in Policies and Procedures (P&Ps), which must match eventual operating conditions (e.g., PCI going forward without on-site surgery) with revised P&Ps. Other long-lead time items might include:
- Certification for PCI without on-site surgery (which in California for example, represents a twelve plus month process).
- Notification of the cardiac surgical group and consideration of all relevant contractual issues.
- Notification and planning for operating room, recovery areas, and cardiac cath lab staffs, including contingency planning as may be required.
- Notification and discussions with county/city emergency medical service and emergency transport providers relevant to STEMI receiving center designation, referral hospital transfer protocols, and the like.
All impacts need to be identified and a plan put in place to mitigate these impacts through a systematic process that specifies identified actions, responsible parties, timeframes required and resources needed. At the conclusion of the Plan development, we strongly recommend it be reviewed and approved by the ESG so all affected parties are informed and the planned-for actions are sufficiently transparent.
Step Two: Unwind Plan Roll-Out
Step Two consists of the roll-out of the Unwind Plan (UP). CFA typically utilizes a project tracking system (Project Tracker) consisting of a Gantt-chart customized with all identified tasks, task assignments, due dates and other relevant information so that project management can be handled efficiently and effectively. After reviewing all assignments with the project team membership, the Project Tracker is approved by the ESG and work initiated. Any required changes in licensing and/or certification will be coordinated with the state licensing bureau and sequenced with the Unwind Plan. For example, under typical circumstances, application for certification for PCI without on-site surgery (and thus discontinuation of cardiac surgery) would come when the Application process is complete and certification approved. Local circumstances and state regulation will dictate the timing and notification of discontinuation and certification or approval of substitute services as needed. Sequencing of “go-live” dates and or “discontinuation” dates will be part of the UP.
Implications
Low-volume cardiac surgery programs are challenging in today’s competitive environment. Hospitals that have gone through the process of evaluating their options, ranging from investment in program development to divestiture or closure, and have decided on the latter strategy, are urged to engage in a systematic and planned process to unwind the cardiac surgery service. Cardiac surgery is impactful to both the overall hospital and the cardiovascular service line, and must be carefully managed, even if that management means unwinding the program.
If you are interested in learning more about strategies to deal with low-volume cardiac surgery programs and/or programmatic assessment for cardiovascular services, please contact CFA at (949) 443-4005 or by e-mail at cfa@charlesfrancassociates.com.