In a previous blog, I posted about the new opportunities for hospital cardiovascular programs to seek “whole program” accreditation or certification from outside validating organizations. This blog post looks at the strategy implications of pursuing such accreditation options.
In a previous blog, I posted about the new opportunities for hospital cardiovascular programs to seek “whole program” accreditation or certification from outside validating organizations. This blog post looks at the strategy implications of pursuing such accreditation options.
It is an obligatory practice in the hospital world to obtain enterprise accreditation as a deeming authority for Medicare certification. Thus, there is a direct linkage between accreditation and reimbursement, and a simple and direct relationship impacting financial performance. Simply stated, get your hospital accredited and certified by Medicare and you can accept their patients, bill and be paid for your services.
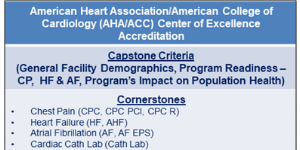
Recently, there have been new efforts by national professional organizations to promote “center of excellence”-based accreditation or certification for entire cardiac programs as well as individual, specialized cardiovascular programs and services. Multiple cardiovascular professional organizations have historically offered specialized clinical service accreditation or certification. However, the trend towards accrediting entire programs is relatively new. CFA applauds these efforts on both conceptual and practical levels.
These new cardiovascular service line accreditation[1] efforts include:
Because cardiovascular accreditation or certification by outside (sometimes competing) experts is not directly tied to payer participation and reimbursement (at least not yet), it must be considered optional. The real question when pursuing accreditation then becomes, “Is it good strategy?” Are the time, effort, and resource commitments required to achieve accreditation really worth it? Will there be a tangible payoff in the future? Is it a valid means to an important endpoint? Is this a defensive or offensive strategy? Or could it be both? Here are CFA’s summary thoughts on the issue.
- Know what you want to achieve with accreditation or certification – Accreditation is a means to an end; that end being third-party validation, enhancement of brand awareness, competitive positioning, and overall enhanced patient care. Certification of individual services or program components may be valuable as a tool to focus needed attention on program development and enhancement of operational or clinical results. Outside readiness assessments, focused on accrediting body requirements, can be a valuable tool to establish and reach consensus on best-practice standards and operational requirements that need to be implemented at your hospital. The internal process required to reach a team-based consensus on these critical issues is always inherently valuable but will take time, commitment, leadership and a commitment of resources to accomplish.
- The pursuit of excellence should always be the superordinate strategy – When discussing this topic, the underlying question has always been; “what is excellence, who defines it, how/by whom is it bestowed, and what does your program need to do to achieve excellence through outside validation?” CFA has always believed that the pursuit of center-of-excellence (COE) status, bestowed by independent third parties or otherwise, is a valuable strategy and for some programs (particularly many low-volume, financially challenged cardiac surgery programs), literally a survival strategy. We have written and consulted on this topic extensively and will continue to do so.
Our own philosophy is that COE status requires that cardiovascular programs meet or exceed high levels of overall performance. While both The Joint Commission and ACC/AHA models address a wide variety of COE characteristics, they focus on the programmatic components that systematically support achieving high levels of a combination of clinical outcomes and a commitment to overall cardiovascular health (i.e., population health). CFA’s COE criteria, accounts for these components, gives appropriate weight to clinical issues, but also acknowledges the need, for example, to achieve high levels of financial and payment-model performance, which is not otherwise addressed by The Joint Commission and ACC/AHA (or other primarily clinically-focused accreditation models) except in broad conceptual terms.
- Overall program accreditation trumps individual service certification – While it may be important to improve the overall performance of an individual service by seeking certification, cardiovascular programs are generally developed and marketed as a whole and not in component parts. After all, a primary goal of such efforts must be to maximize brand awareness and strategic positioning, typically through brand awareness and overall positioning. Accreditation of an entire program should produce greater long-term results and a bigger bang-for-the-buck than certification of an individual service simple due to its comprehensive, building-blocks of excellence, approach. Therefore, if a commitment is made to pursue program accreditation as a strategy, it will potentially be more valuable, by coordinating all programs and services together, placing an emphasis on perfecting a uniform “system of care,” than certification of an individual, specialty service.
For example, does having a certified cath lab mean you have a cardiovascular center of excellence? This should not be taken as denigrating the need to improve individual service components if that is necessary and/or supported by specific physicians interests or efforts, after all, the cardiovascular program is no stronger than the individual services that go to make up the whole service line.
- Accreditation should be viewed as part of an overall population health strategy – One important premise behind whole-program accreditation programs is the fundamental, underlying commitment to improving a community’s cardiovascular health. For a hospital, this commitment was historically supported (to a greater or lesser degree) by education, screening and risk-assessment programs for the community. As fundamental care provision changes and as analytic capabilities and payment incentives continue to evolve, hospitals will expand their population health capabilities to include a focus on cardiovascular health. The accreditation processes that focus on the building blocks of preventative care, diagnostic and treatment services through an episode of care focus (and resultant payment incentives/disincentives), will strengthen a hospital’s capabilities and support its commitment to population health as a going-forward strategy through building a comprehensive system of care.
- Choose wisely between competing accreditation organizations – Complicating matters is the fact that both The Joint Commission and AHA/ACC have competing center-of-excellence accreditation programs. Is one better than the other? Will one produce the desired results more effectively or less expensively? How will competing models be received by the target community(ies)? Because all of this is relatively new, it is simply too early to tell if one approach is favored in the market over the other. Remember also that there are other professional societies that offer individual service certification. Physicians may prefer the AHA/ACC model, while hospital administration may prefer The Joint Commission model because of their familiarity with the current hospital accreditation organization and process. It will be important that the cardiovascular program team decide which approach best suites its goals and objectives and seek a consensus on approach. Gaining solid physician support should not be underestimated; therefore, the AHA/ACC model may have a credibility edge with the medical staff.
There seems little question that accreditation/certification should be on the agenda for every hospital cardiovascular program in the near to mid-term future. As a developmental strategy, it has real merit and makes logical sense for many hospitals, particularly in highly competitive markets. It does require a certain “leap of faith;” that the effort and resources required to achieve validated status will stimulate a hospital’s cardiovascular service line in its quest for center of excellence status and ultimate, on-going success in the marketplace. It also begs the question of how successful a population health approach will fare in the local evolving healthcare marketplace. Carefully consider all of the options, discuss this strategy in detail, and make a consensus-based decision that is right for your health system, your hospital, your cardiovascular service line and unique market situation.
We will be posting additional articles regarding center of excellence development and program accreditation/certification in the near future.
If you are interested in learning more about strategies to deal with accreditation/certification, low-volume cardiac surgery programs and/or programmatic assessment for cardiovascular services, please contact CFA at (949) 443-4005 or by e-mail at cfa@charlesfrancassociates.com.
Footnotes
[1] For purposes of this discussion, we make no distinction between the use of the terms “accreditation” and “certification.”

 In a previous blog, I posted about the new opportunities for hospital cardiovascular programs to seek “whole program” accreditation or certification from outside validating organizations. This blog post looks at the strategy implications of pursuing such accreditation options.
In a previous blog, I posted about the new opportunities for hospital cardiovascular programs to seek “whole program” accreditation or certification from outside validating organizations. This blog post looks at the strategy implications of pursuing such accreditation options.