Rethinking Ambulatory Cardiovascular Strategy: Part One – The Big Picture
Sometimes being a California company lulls one into a false perception of normalcy. Because of the...
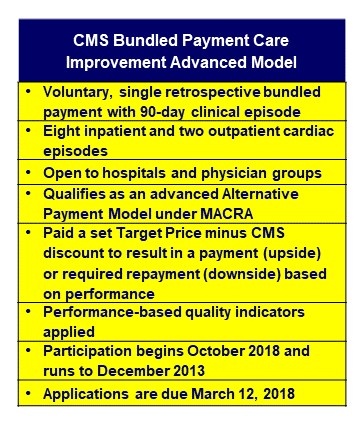
Following our posting of the blog announcing the CMS Final Rule ending the proposed Mandatory Cardiac Bundled Payment initiative posted on December 5, 2017, a little over one month later, CMS announced its new voluntary bundled payment model (see CMS Announces New Voluntary Bundled Payment Model for Ten In- and Out-Patient Cardiac Clinical Events, posted January 10, 2018.)
After these events, CFA was engaged in a conversation with a cardiac service line administrator of one of the largest programs in the Western U.S. When we mentioned the formal cancellation of mandatory cardiac bundles, this person asked a key question about the new CMS voluntary bundle initiative process – “Why would we want to do that?” Frankly, given CMS’s recent webinars and proliferation of documents on the bundle, we are asking the same question! As is often the case, the simplest most direct question often gets to the true heart of the matter. With all the discussion (and our own past blog posts) on this subject, we are sure that this question will be asked repeatedly. Just as a point of reference, CMS had over 600 questions submitted for its first webinar on the subject. Since that initial client conversation, CMS announced January 9th the new voluntary advanced bundled payment model that includes ten cardiac episodes (see table). 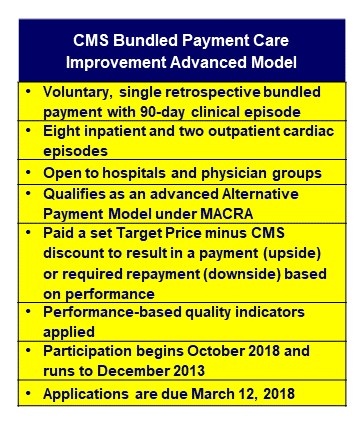 Given the proposed March 12, 2018 deadline to apply for the new bundle, the question asked becomes not only relevant, but also timely and challenging[1] to answer.
Given the proposed March 12, 2018 deadline to apply for the new bundle, the question asked becomes not only relevant, but also timely and challenging[1] to answer.
In thinking about an answer to this question, particularly in light of the CMS announcement, CFA offers the following for all to consider.
Therefore, the announcement of the new advanced bundle should not have been a surprise, but the rapidity with which they are proceeding clearly caught many off guard, as did the overall complexity involved, as did the March 12 application due date. As with many things CMS proposes this date may be pushed back depending upon demand and industry pushback.
The documented facts prove that bundles have worked in the past – lowering costs and enhancing outcomes – and will likely work in the future. CMS is moving to bundles. The ten cardiac episodes listed in the Request for Applications (RFA) cover a significant percentage of any program’s cardiac volume, especially procedural volume. CFA has always believed that bundles in the form of a defined CMS innovation process looking to identify “best practice models” across the spectrum of hospital operating environments, was inevitable and represents a clear direction for the future2.[2]
A potential key “value-add” for CMS, hospital executives, physicians and clinical staff is creating a process that clearly incentivizes simplifying and streamlining delivery processes (reduced overall burden of care delivery) driven by engaged stakeholder physician-driven teams. In our experience, this would get to the heart of the “Why would we do this?“ question by making the goal not only better clinical outcomes and cost reduction, but enhanced physician satisfaction too. This potential innovation objective would require hospitals and physicians to develop an “overall satisfaction” metric in the new bundled process. While trying to standardize physician satisfaction is not an easy proposition for sure, acknowledging it and developing a qualitative measure of the physician experience can strengthen the program. These measures can include the level of technologic and operational process frustration expressed by the physicians and could help drive improvement with inefficient clinical processes and redundant or unnecessary administrative tanks that are so challenging to physicians and often impact their willingness to innovate. We believe, based on previous CMS guidance, this is a metric they want or will want measured.
It will be interesting to see what type of response CMS receives on March 12. If too few applications are received by the deadline, will they extend it? Clearly, a read of the RFA document shows that hospitals that have either prepared for or actively participated in previous CMS bundled payment models have an advantage based upon their collective experience and the supportive infrastructure and processes they have developed. Hospitals new to bundling but who perceive the new model as an opportunity will need to scramble to make the March 12 deadline (unless CMS pushes back the filing date) and may be at a disadvantage if this application process is truly competitive. Nevertheless, every hospital should carefully consider its options, evaluate the risk/reward equation, and its readiness to participate in this specific bundling opportunity or the next. Surely, there will be a next.
If you are interested in learning more about strategies to deal with bundled pricing, cardiac services strategic development, service expansion or low volume cardiac surgery programs and/or other programmatic needs for cardiovascular or other services, please contact CFA at (949) 443-4005 or by e-mail at cfa@charlesfrancassociates.com.
[1] A particular challenge involves participants (both hospitals and physician group practices alike) choosing to become “Convener” or “Non-Convener” participants with implications for bringing together multiple downstream entities or “Episode Initiators.”
[2] It is assumed, but has yet to be confirmed, that non-participating hospitals will continue to be paid existing fee-for-service rates until some future date when Medicare revises its current payment system.

Sometimes being a California company lulls one into a false perception of normalcy. Because of the...

The last few years have been financially devastating for the hospital industry. COVID-19 and its...