Study Demonstrates that the U.S. AMI Rate Is Decreasing
A recently published study purports to show that the incidence of acute myocardial infarction (AMI) in the US has decreased over the nine-year period between 1999 and 2008.
A Cardiovascular Consulting Blog from CFA
Posts about:
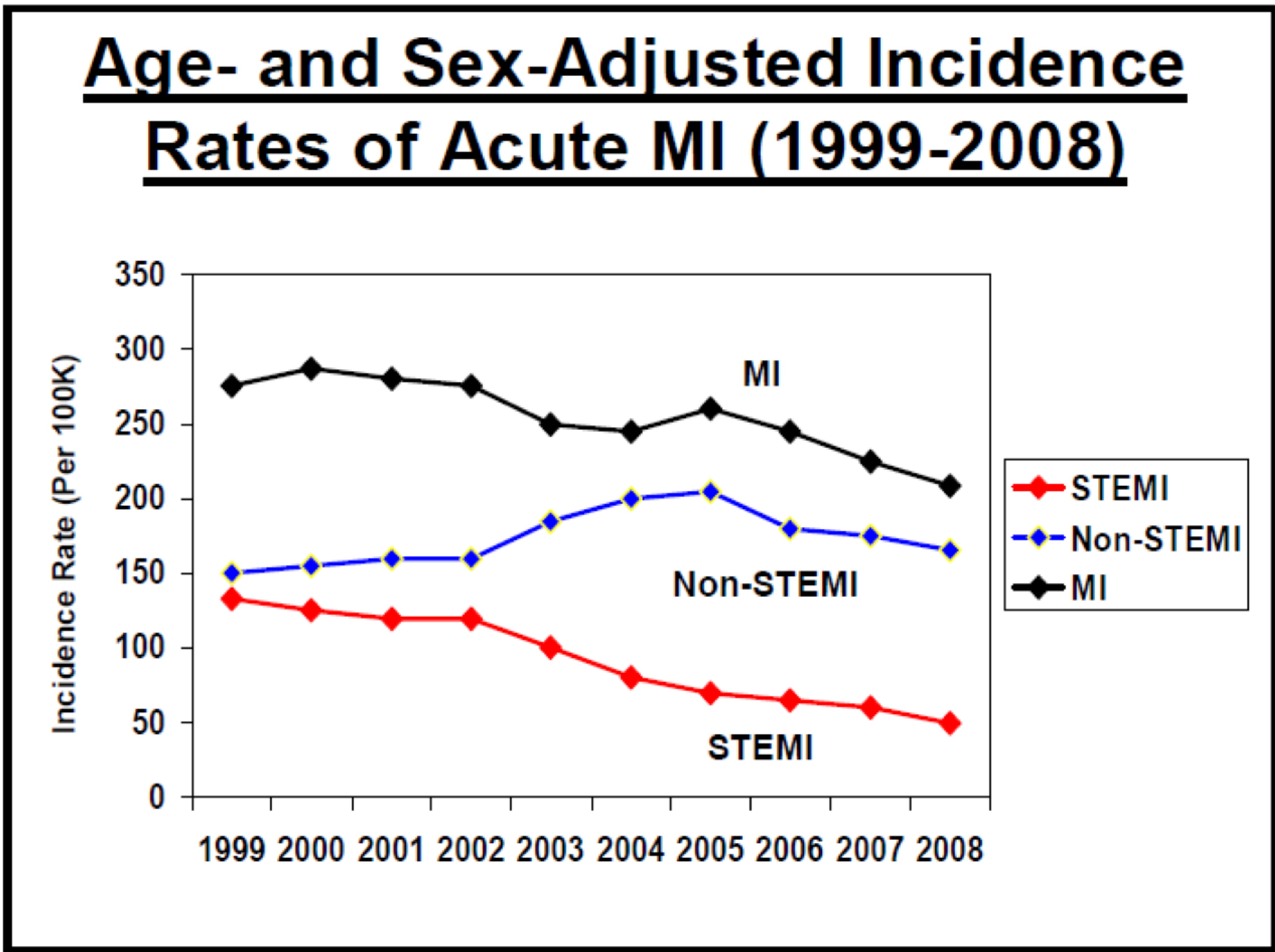
A recently published study purports to show that the incidence of acute myocardial infarction (AMI) in the US has decreased over the nine-year period between 1999 and 2008.
Continuing the discussion from Part One of physician/hospital alignment and the reemergence of bundled payment initiatives, let’s discuss the impact of health care reform in the area of bundled payment for care. A national pilot program on payment bundling is included in H.R. 3590, the Patient Protection & Affordable Care Act. This pilot program is set to commence in 2012 (no later than January 1, 2013) and run for five years.
