Cardiovascular Center of Excellence Accreditation Opportunities Expanding
Late last year, the opportunity for hospital cardiovascular (CV) programs to seek “whole program”...
FFR-CT Aims for Real-World Application
Fractional flow reserve-computed tomography (FFR-CT), in the still early stages of clinical implementation, is beginning to make inroads into how some hospitals and physician groups diagnose chest pain patients noninvasively.
Some cardiologists have described it as a “paradigm shift.” Early adapters have seen declines in cath lab admissions and changes in the way they approach the diagnosis of obstructive coronary artery disease. FFR-CT accomplishes something that no other methodology has been able to – noninvasively; providing both an anatomical and a functional assessment (e.g., actual blood flow). It could potentially replace catheter-based, invasive FFR pressure wire measurements in many patients. It could save money and time by reducing the need for additional tests, facilitate early discharge of chest pain patients without coronary occlusions, and reduce/eliminate coronary angiograms. As with the roll-out of virtually all new technologies, there remains many questions about its optimal clinical use and concomitant organizational implications
Current Practice
Currently, there are various alternative methods used to diagnose suspected coronary artery disease – none of them perfect – all with limitations. Invariably, regardless of diagnostic method, many patients end up in the cath lab for invasive angiography and potentially a catheter-based FFR procedure. Various studies have documented the fact that too many patients go to the cath lab and are diagnosed with clinically insignificant coronary artery disease, leading to overutilization, clinical risk and high cost. Cardiac CT provided a significant anatomical view of the coronary vessels, but falls short on evaluating “intermediate” lesions – those that are truly dangerous (typically with blood flow capacity limited to 40 to 70 percent). Dealing with the intermediate lesions (particularly when multiple intermediate lesions are present) is the primary niche of FFR-CT.
The New Technology
FFR-CT is the exclusive domain of HeartFlow® which provides proprietary software that collects data sent from the user, analyses the data and calculates the results, and transmits the results back to the user. The technology is extensive, including the use of proprietary algorithms, artificial intelligence, supercomputers, and highly trained staff. The delay in results (currently a matter of hours), is a primary disadvantage to its use, particularly for emergency department cases. Although, it should be noted, that anecdotal information says that some hospitals are using HeartFlow® analysis for chest pain patients in the ED. (For a full description of the product, go to www.heartflow.com). The U.S. Food and Drug Administration (FDA) cleared FFR-CT in November 2014, and it is currently reimbursed through Category III CPT codes for Medicare and many commercial payers. It is currently approved in the U.S., Canada, Europe and Japan.
The technology has been validated through a number of clinical trials, most prominently the PLATFORM trial and RIPCHORD study in Europe. It has been presented at the annual American College of Cardiology and Society of Cardiovascular Computed Tomography meetings. PLATFORM revealed that 61 percent of patients did not need invasive coronary angiography, resulting in a 32 percent lower cost. In RIPCHORD, three experienced cardiologists reviewed coronary CT angiography images of 200 patients with stable chest pain and agreed on one of three treatment options: optimal medical therapy, PCI or bypass surgery. The physicians were then shown FFR-CT analysis for each patient and asked to make a second treatment decision. In total, viewing the FFR-CT analyses resulted in a change in treatment plan for 36 percent of patients. Also, in 18 percent of cases initially decided for PCI, one or more target lesions were changed following FFR-CT analysis.
Currently FFR-CT is available to only a fraction of potential patients in U.S. hospitals, free-standing CT centers and/or radiology or cardiology medical groups. In a review of the HeartFlow® website for example, in California, there were three hospitals, one radiology group location, one cardiology group, and a research institute listed as available providers.
Patient Selection
Patient selection remains the single biggest issue with implementation of FFR-CT. As referenced above, intermediate lesions remain the target for further evaluation. If CT angiography identifies clearly high-level, multi-vessel disease, or the opposite, smaller lesions unlikely to have a significant impact on blood flow, treatment decisions are relatively clear cut. FFR-CT can help to identify intermediate (particularly multiple) lesion severity and prioritize the most significant. Another issue is that, unlike clinical practice in many European countries, cardiac CT is not the typical first line of diagnosis for chest pain patients (in comparison to, for example nuclear myocardial perfusion imaging) – largely due to insurance issues. In some European settings, virtually all chest patients are referred for CCT, and FFR-CT analysis is used for all patients with intermediate lesions of 40 to 70 percent stenosis. American cardiologists continue to develop FFR-CT and its application to patients. Limitations are currently few, including the inherent delay in receiving the analysis from HeartFlow®, and limitations based on the precision of the CT images (false positives are still a risk).
Experience at California Pacific Medical Center
One early adapter has been California Pacific Medical Center in San Francisco, a large, urban full-service cardiovascular provider. Opening new facilities with 256-slice CT capability and support from a radiology champion served as their incentive to partner with HeartFlow™. According to W. Michael Barber, R.N., Manager of Cardiac Cath Labs, Interventional Radiology and Electrophysiology, early results are very promising. “It’s hard to find anything negative about this technology,” he says. FFR-CT’s utilization at this hospital is increasing rapidly as more cardiologists accept its clinical utility under specific (albeit still evolving) circumstances. While the technology is designed to produce definitive results to prevent further testing, from nuclear stress testing to diagnostic (or potential therapeutic) catheterization, he believes that broad adoption could actually lead to increased cath lab utilization, as patients that truly need revascularization through PCI are definitively identified. CPMC has a high volume of emergency department presentations, as well as critical care transfers from outlying hospitals, which complicates the decision-making surrounding the use of FFR-CT. Optimization of results analyses turnaround times from HeartFlow™ remains a key goal, given that application to specific patients (and results turnaround times) is highly variable and active roll-out of the methodology continues. A consensus-based treatment protocol is currently being developed to identify appropriate candidates, standardize both the process and the treatment required to optimize usage and mitigate delays. The additional fact that the technology is well reimbursed is also a positive in its adaption.
Outstanding Issues Going-Forward
As with the roll-out of virtually all new technologies, there remains many questions about its optimal clinical use and concomitant organizational implications. Among these questions are the following:
Conclusion
Like many developing technologies, FFR-CT has a tremendous upside potential in diagnosing the significance of a patient’s coronary artery disease. This potential can only be reached through broad, universal adaption and the mitigation of existing barriers and limitations (perceived or real). Significant barriers still exist that will slow adaption and prevent its potential from being reached. It is incumbent on all hospitals with cardiovascular programs to critically evaluate this technology and objectively determine its place in the unique program and service offerings for each hospital and each unique marketplace.
If you are interested in learning more about any of this important issue or in cardiac services strategic development, service expansion and/or other programmatic needs for cardiovascular or other services, please contact CFA at (949) 443-4005 or by e-mail at cfa@charlesfrancassociates.com.
[1] Douglas, PS, et al. One-Year Outcomes of FFR-CT-Guided Care in Patients with Suspected Coronary Disease: The PLATFORM Study. J. American College of Cardiology, 2016; 68(5): 435-45.
[2] Douglas, PS, et al. Clinical outcomes of fractional flow reserve by computed tomography angiographic-guided diagnostic strategies versus usual care in patients with suspected coronary artery disease; the prospective longitudinal trial of FFR (CT); outcomes and resource impacts study. European Heart Journal 2015; 36(47): 3359-67.
[3] Believed to be helpful, but not mandatory.
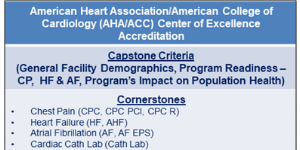
Late last year, the opportunity for hospital cardiovascular (CV) programs to seek “whole program”...
Three-dimensional imaging diagnostics-in particular, Cardiovascular CT angiography (CCTA)-have been...