Low-Volume Cardiac Surgery Programs: Cardiac Valve Surgery Trends and Implications
CFA has written extensively on the challenges facing the low-volume cardiac surgery program.

 Hospitals with small to medium-sized cardiac valve surgery programs need to know that the era of TAVR for most or all aortic valve replacement cases (AVR) – regardless of overall risk category – is moving ever closer to reality.
Hospitals with small to medium-sized cardiac valve surgery programs need to know that the era of TAVR for most or all aortic valve replacement cases (AVR) – regardless of overall risk category – is moving ever closer to reality.
A recently published clinical trial of low-risk TAVR patients did not find any significant differences in the rate of all-cause mortality between low-risk patients undergoing TAVR and a control group undergoing surgical aortic valve replacement (SAVR).[i] Positive results for high-risk, then medium-risk, and now low-risk patient cohorts would suggest that the clinical appropriateness of TAVR for all or certainly the majority of patients requiring AVR is now one step closer to becoming best practice.
Recognizing that regulatory and reimbursement changes historically lag behind both clinical trial outcomes and professional society guidelines and recommendations, hospitals with cardiac valve surgery programs will need to evaluate their program volume and SAVR/TAVR procedure mix as the dust finally settles on both clinical appropriateness and reimbursement-related issues. Consequently, low-volume cardiac valve surgery programs are rapidly approaching a crossroads where strategic decisions will need to be made if program viability is at stake in those markets where higher-volume TAVR providers take more volume away from existing non-TAVR providers. In the future, a hospital left with only SAVR capability will be at a distinct disadvantage.
The Current State
CFA has blogged extensively on TAVR-related issues and strategy. Here is a recap of important past and current information, followed by strategic implications.
Strategic Implications
On the surface, the broadening of clinical indicators for TAVR to include nearly all patients requiring AVR, has the potential to reconfigure local marketplaces. This should allow the average TAVR provider to increase its volume and thus come closer to meeting or exceeding the national minimum volume standards – especially if minimum thresholds are decreased. It may also allow some lower volume providers to establish TAVR programs for the first time. Lowering of the volume standard by Medicare would potentially assist this scenario. Low-volume cardiac valve surgery programs will now be faced with a complete loss of AVR surgery cases, potentially putting an additional strain on overall program volume and forcing them to make hard decisions about program viability and financial performance.
In our last related blog post, we commented on the need for any hospital contemplating entering this market to think long and hard before making a decision. Optimizing TAVR programs specifically, and valve surgery programs in general, has been challenging even in high-volume situations. The potential for virtually all AVR candidates to receive TAVR at approved centers certainly needs to be factored into every hospital’s unique market and circumstances. Increasing the overall surgical volume may very well help some programs achieve a degree of viability, but careful consideration of potential volume, reimbursement, competitive position, cost and associated factors will be needed to make a robust strategic decision going-forward.
If you are interested in learning more about low-volume cardiac surgery program strategies and options, please download our updated and expanded whitepaper (see Low-Volume Cardiac Surgery Programs: Grow, Consolidate or Divest: Self-Preservation Strategies and Excellence Expectations, our expanded and updated White Paper). If you are interested in cardiac services strategic development, service expansion and/or other programmatic needs for cardiovascular or other services, please contact CFA at (949) 443-4005 or by e-mail at cfa@charlesfrancassociates.com.
Footnotes
[i] Waksman, Ron, et al, Transcatheter Aortic Valve Replacement in Low-Risk Patients with Symptomatic Severe Aortic Stenosis, JACC: August 2018, DOI: 10.1016/j.jacc.2018.08.1033
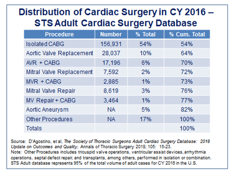
[ii] D’Agostino, et al, The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2018 Update on Outcomes and Quality, Annals of Thoracic Surgery, 2018; 105; 15-23.
[iii] Grover, F. L., and Holmes, D. R., New Insights from the STS/ACC TVT Registry, Cardiac Interventions Today, Vol. 11, No. 2, March/April 2017.
[iv] Galewitz, Phil, Hospitals Battle For Control Over Fast-Growing Heart-Valve Procedure, Kaiser Health News, posted online August 17, 2018.
CFA has written extensively on the challenges facing the low-volume cardiac surgery program.
CMS announced its long-awaited updated transcatheter aortic valve replacement (TAVR) national...