Over the last few years, there has been a keen interest in the patient-centered medical home (PCMH) model of care, highlighted by its prominent inclusion in the Patient Protection and Affordable Care Act (PPACA).
The framework for the model was created years ago by the American College of Physicians and endorsed over time by many professional societies and medical professional associations including the American College of Cardiology (ACC). It has also been promoted by labor unions, health plans, consumer groups and large businesses. The Commonwealth Fund has identified seven attributes necessary for patient-centered care:
- Access to care;
- Patient engagement;
- Clinical information systems that support high-quality care, practice-based learning and quality improvement;
- Care coordination;
- Integrated and comprehensive team care;
- Routine patient feedback to doctors; and
- Publicly available information.
The above attributes sound like logical and commendable goals that any physician practice should strive for. The problem is in the details, and ultimately, in what physicians get reimbursed. The PCMH model is viewed almost universally as a primary care-centric model, although who constitutes a “Primary Care Practitioner” is currently not well defined. How do specialists fit the model? It assumes that internal medicine-trained specialists such as cardiologists, although capable of being the principal physician in a PCMH model, would not readily choose this role. Specialists are justifiably concerned that reimbursement dollars will be shifted away from their specialties towards primary care under a fully-implemented PCMH model. Additionally, the treatment of chronic medical conditions figures prominently in coverage plans and therefore impacts specialists like cardiologists who are expert in treating chronic illnesses such as advanced congestive heart failure and chronic cardiac arrhythmias. Key question; how many “primary care” patients do cardiologists see in their practices? Is the PCMH concept for these specialists even an issue?
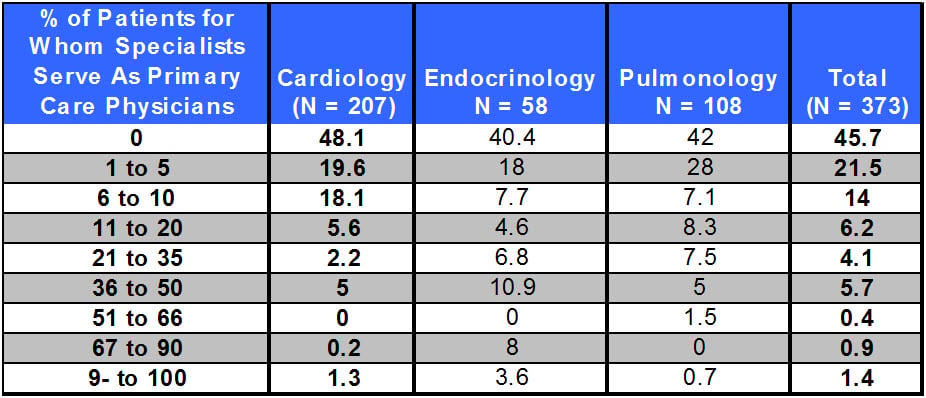
Research suggests it may not be an issue at all. The New England Journal of Medicine published Specialist Physician Practices as Patient-Centered Medical Homes, in April 2010, in which they conducted a tel ephone poll of selected specialists (including 207 cardiology practices) to answer the question, “…for approximately what percentage of patients, if any, do the physicians in your practice serve as primary care physicians as well as specialists?” In 86% of surveyed cardiology practices, physicians served as primary care practitioners for 10% or fewer patients. According to their own report, the overwhelming majority of cardiologists provide primary care for very few or none of their patients. However, a minority do provide some amount of primary care. Please see the summary table with this information.
ephone poll of selected specialists (including 207 cardiology practices) to answer the question, “…for approximately what percentage of patients, if any, do the physicians in your practice serve as primary care physicians as well as specialists?” In 86% of surveyed cardiology practices, physicians served as primary care practitioners for 10% or fewer patients. According to their own report, the overwhelming majority of cardiologists provide primary care for very few or none of their patients. However, a minority do provide some amount of primary care. Please see the summary table with this information.
Despite this seemingly minor impact, the ACC has established initiatives to keep cardiologists from being per se excluded from participation as a medical home, including the establishment of the CardioSmart.org website, and the Patient-Centered Care Committee (PC3), charged with “transforming the patient care experience and improving health outcomes for people with heart disease through development of partnerships, programs and tools that support care …” It seems that their fear is twofold: 1) that the model will downplay the role of specialists (to save money); and 2) that PCP’s will manage complex CV-related chronic conditions, to the detriment of the patient and the financial health of the specialist.
Whether or not cardiologists will choose to participate in the Medical Home model is certainly debatable. If they do participate, they will undoubtedly be held to the high standards established for PCPs. This will include the standard of care they now provide, plus …”proactively, systematically and in an organized manner, trying to improve the health of the population of patients within a practice…” using healthcare information technology (sharing data among providers), nurse care managers and other disparate resources. Compliance with these requirements of participation will be a significant challenge for any practice, but particularly challenging to cardiologists and other specialty practices!
CFA invites your comments, suggestions and questions.